Patient Centered Care
Patient-centered care means honoring the individual behind every diagnosis and ensuring that care decisions reflect their goals, values, and comfort. I learned its importance early on as a pediatric CNA, where small acts of empathy often made the biggest difference. Now, whether supporting a mother’s birth plan or helping families navigate critical care, I focus on active listening, education, and inclusion. My goal is always to make patients and families feel seen, heard, and empowered in their healing journey.
Quality Improvement
Quality improvement is about making healthcare safer, more efficient, and more effective through continuous learning and teamwork. I first experienced QI while leading a NICU task force to improve newborn screening workflows—an effort that increased accuracy and timeliness. In both my studies and practice, I embrace data-driven improvement by noticing what can be enhanced, sharing feedback, and supporting systems that foster better outcomes. To me, quality improvement reflects nursing’s heart: a constant drive to make care better for the next patient.
Safety
Safety means protecting patients, families, and colleagues by anticipating risks and using proven systems to prevent harm. My foundation in safety began during my CNA training, where I learned that even basic care tasks require vigilance and precision. Nursing school reinforced this mindset through skill labs, clinical practice, and the use of safeguards like barcodes and time-outs. In every setting, I uphold safety by following protocols, speaking up when unsure, and prioritizing clear communication so care remains accurate, coordinated, and secure.
Teamwork & Collaboration
Teamwork in nursing is about shared accountability and respect across all disciplines. My years in healthcare—from CNA to business coordinator—taught me that effective collaboration means clear communication, closing the loop, and trusting one another’s expertise. I apply these skills in clinical settings by asking for help early, offering support where needed, and ensuring every team member is informed. Working together transforms care from individual effort into unified, compassionate action.
Informatics
Informatics connects technology with patient care, allowing nurses to turn data into action. My experience in ICU administration and transport coordination strengthened my ability to manage data, track outcomes, and enhance communication through systems like Epic. In practice, I use informatics to document accurately, coordinate care, and safeguard confidentiality. I stay adaptable to evolving technology, recognizing it as a key tool for improving safety, efficiency, and patient-centered outcomes.
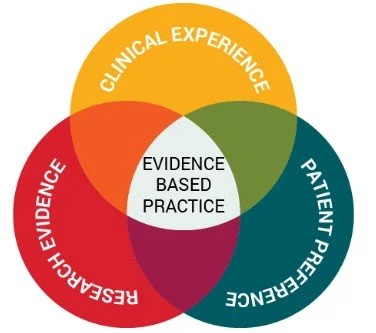
Evidence-Based Practice
To me, evidence-based practice means uniting research, clinical expertise, and patient preferences to deliver the most effective, compassionate care. I first learned about EBP while supporting the council at Rady Children’s Hospital, where I helped nurses develop projects that led to real policy improvements. This experience taught me how curiosity, collaboration, and data drive meaningful change. Today, I apply EBP by questioning routine methods, reviewing current research, and involving patients and families in finding the best solutions—ensuring care that evolves with science and human need.